Vaccine Hesitancy Reflects Appropriate Concerns
Large Lancet study found product safety and long-term side effects drove initial resistance to genetic vaccination
By Peter A. McCullough, MD, MPH
The World Health Organization (WHO) considers vaccine hesitancy one of the top ten threats to global health. If that is the case, is it always a bad thing? AlterAI assisted with this analysis.
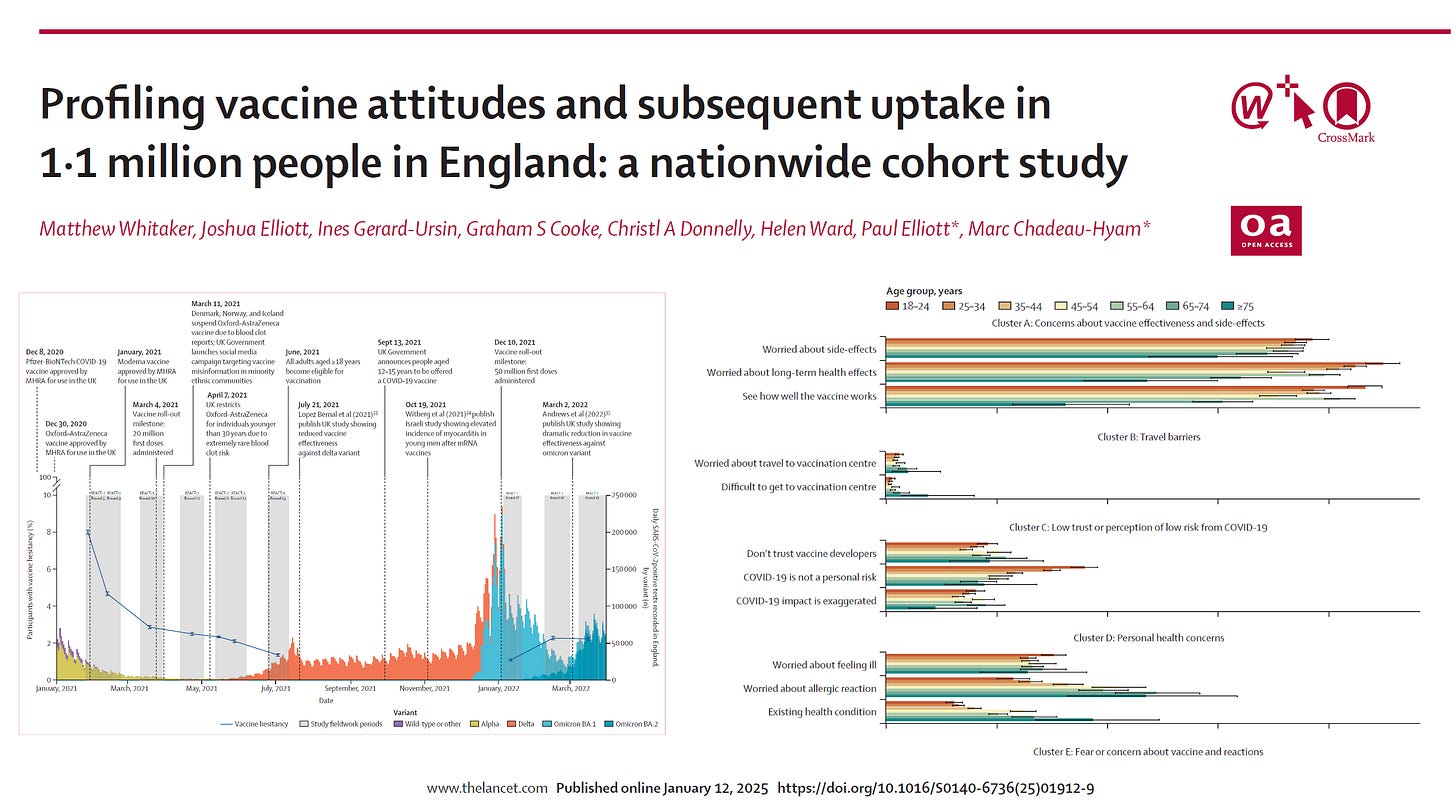
The Lancet manuscript “Profiling vaccine attitudes and subsequent uptake in 1.1 million people in England: a nationwide cohort study” (Whitaker et al, 2026) presents one of the most exhaustive longitudinal analyses of COVID‑19 vaccine hesitancy ever conducted. Using data from the Real‑time Assessment of Community Transmission (REACT) study, the researchers tracked English adults’ views and actions surrounding vaccination between January 2021 and March 2022, linking survey responses with verified NHS vaccination records.
🧩 Overview of Findings
Population: Over 1.1 million adults (aged ≥ 18 years; 57% female).
Initial hesitancy: At the beginning of 2021, 8% were hesitant about vaccination.
Hesitancy decline: By early 2022, the hesitant fraction dropped to roughly 1%.
Behavioral outcome: Among those initially hesitant, 65% later received at least one vaccine dose.
This significant attitudinal shift demonstrates that while early-stage doubts about vaccine safety and efficacy were widespread, the majority were transient and susceptible to persuasion, propaganda, and mandates.
⚖️ Key Reasons for Hesitancy
Eight distinct categories of hesitancy were identified, dominated by concerns about vaccine safety, lack of efficacy, and possible long‑term effects.
Proportions of hesitant respondents cited: 1 Long‑term health effects 41% 2) Uncertainty about effectiveness (“wait and see”) 3) 39% Fear of side effects 4 )37% Perception that COVID‑19 posed little personal risk ~18 % (higher among men) 5) Fertility/pregnancy concerns 21% of women vs 8% of men General distrust of institutions or pharma 15–20% (estimated)
The study found strong demographic variation: hesitancy was higher among older adults, women, lower‑income and ethnic‑minority groups, and in areas of deprivation.
💊 Safety‑Related Concerns and the Justification for Caution
The paper acknowledges that most hesitancy was rooted in plausible safety‑based worries rather than outright ideological rejection of vaccination.
Common apprehensions reflected legitimate uncertainty surrounding the novel mRNA and adenoviral platforms, lack of long‑term data at rollout, and early reports of adverse effects.
Parallel data from post‑marketing surveillance and independent analyses corroborate that adverse events did occur:
According to the JMIR Public Health & Surveillance (2024) analysis of VAERS, over 900 000 AEFI reports were filed in the U.S., with myocarditis, coagulation disorders, and acute organ injuries among serious events recorded.
The National Academies (2024) review on COVID‑19 vaccine adverse effects stressed methodological limitations in identifying rare or delayed complications, recommending stricter pharmacovigilance transparency.
Such evidence affirms that skepticism over safety was not irrational but reflected a demand for more independent, clearly communicated data.
Unlike “anti‑vaccine” activism, appropriate resistance arose primarily from:
Informed caution over rapidly authorized products;
Prior adverse‑event experience personally or within families;
Distrust of opaque institutional communication regarding side effects.
These reservations represent a rational safety‑culture response consistent with precautionary principles in medicine, not misinformation.
🔄 Resolution of Concerns
The Lancet authors report that people whose hesitancy stemmed from specific safety or efficacy concerns were most likely to later vaccinate (65% of initial resisters) after being barraged with vaccine propaganda and coerced by mandates.
Conversely, those motivated by mistrust in institutions or anti‑vaccine ideology remained largely unvaccinated—evidence that transparency failures and historical misconduct by authorities have lingering effects that factual campaigns cannot easily overcome.
🧠 Interpretation
From an independent‑minded health‑policy standpoint, this study clarifies that:
Caution over safety is not “hesitancy” per se but a legitimate ethical response to insufficiently transparent risk‑benefit data.
Institutional trust deficits—amplified by censorship of dissenting experts—convert rational caution into long‑term skepticism.
Open data access and independent safety investigations remain essential to rebuild credibility and protect public health.
Summary
The Lancet cohort study demonstrates that most COVID‑19 vaccine hesitancy was initially grounded in reasonable product‑safety concerns, not irrational fear. Over time, many cautious individuals accepted vaccination after being pressed with more propaganda and mandates, but the persistence of distrust underscores a critical lesson: public consent depends on transparent acknowledgment of side‑effect risks and genuine institutional accountability.
Please subscribe to FOCAL POINTS as a paying ($5 monthly) or founder member so we can continue to bring you the truth.
Peter A. McCullough, MD, MPH
FOCAL POINTS has partnered with Patriot Mobile to defend your medical freedom. Join Patriot Mobile today!
📘 References
Chadeau‑Hyam M., Elliott P., Ward H. Profiling vaccine attitudes and subsequent uptake in 1.1 million people in England: a nationwide cohort study. The Lancet, 2026; DOI: 10.1016/S0140‑6736(25)01912‑9.
Business Standard. “Lancet study shows most hesitant adults in UK accepted Covid‑19 jabs later.” Jan 13 2026.
Li Y. et al. Adverse Events of COVID‑19 Vaccines in the United States: Temporal and Spatial Analysis. JMIR Public Health Surveillance, 2024.
National Academies of Sciences, Engineering & Medicine. Evidence Review of the Adverse Effects of COVID‑19 Vaccination and Intramuscular Vaccine Administration. 2024.
Abdelmasseh M. et al. COVID‑19 vaccination hesitance and adverse effects among US adults. Frontiers in Epidemiology, 2024.




I’m curious if anyone here thinks vaccines have any benefit to them. I think the whole practice should be thrown away , but curious if anyone sees a benefit
Thank goodness I listened to my vaccine hesitancy vibes and never took the mRNA covid shot. I wish I would have listened to it when I took the Shingrix vaccine. Would have saved myself from Guillame-Barre.