What is the Smallest Worthwhile Difference in Cardiovascular Risk?
Novel measure tested for public acceptance of statin therapy
By Peter A. McCullough, MD, MPH
Despite dozens of high quality trials, mechanistic studies, and widespread generic availability, there remains great resistance to oral statins to reduce the risk of athersclerotic cardiovascular risk (myocardial infarction, stroke, need for revascularization, and cardiovascular death). Alter AI assisted with this interesting paper from Japan.
The study “Measuring Public Preferences for Statin Therapy Using the Smallest Worthwhile Difference” (JAMA Internal Medicine, published online February 16, 2026) by Luo et al. explored how laypeople in the United States and Japan evaluate the benefits and burdens of statin therapy for primary prevention of atherosclerotic cardiovascular disease (ASCVD). Although clinical guidelines strongly recommend statins to reduce cardiovascular risk, these guidelines are based on expert judgment, whereas patients’ own preferences and thresholds for perceiving benefit remain poorly understood. The investigators applied an explicit decision-making metric—the Smallest Worthwhile Difference (SWD)—defined as the minimum absolute risk reduction in ASCVD events that individuals consider sufficient to justify long-term statin use.
Methods:
Online surveys were administered to adults aged 40 to 75 years with no prior statin use. The samples—254 U.S. respondents and 297 Japanese respondents—were recruited through research panels using stratified sampling to approximate national demographics. Participants were educated about statin benefits and side effects, completed comprehension checks, and then answered iterative trade‑off questions using graphical displays. Each person reported the absolute risk reduction they would require to consider statin therapy worthwhile under three baseline 10‑year ASCVD risk scenarios: 2%, 10%, and 20%. The usual threshold for a doctor to recommend a statin is a 10-year actuarial risk of 10%. Most patients with 20% risk have already manifested atherosclerosis. Actual statin efficacy was provided as approximately a 25% relative risk reduction per 38.6 mg/dL decrease in LDL cholesterol (roughly a 2–3% absolute reduction) over two years.
Findings:
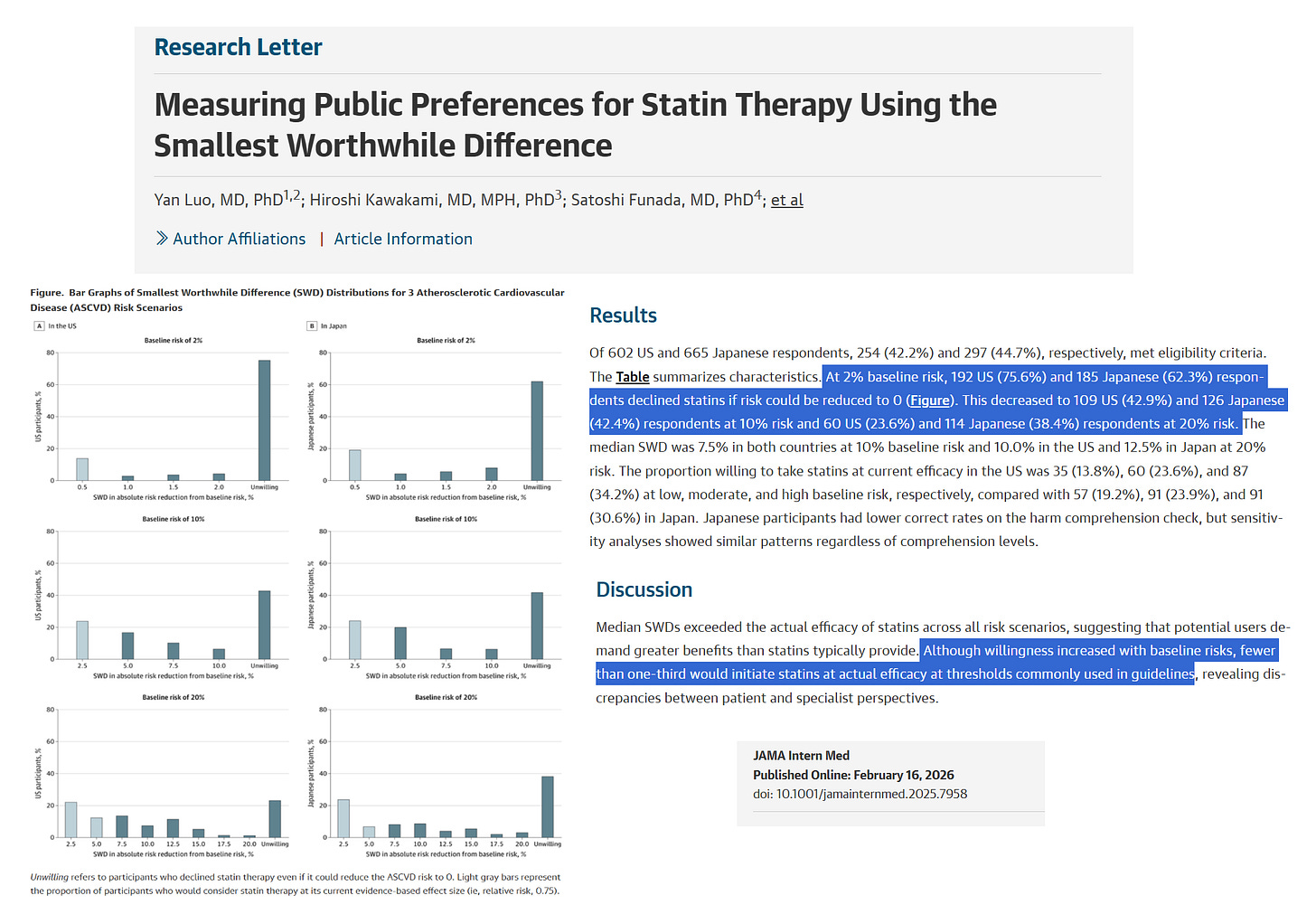
At a 2% baseline risk, 75.6% of U.S. and 62.3% of Japanese participants refused statins even if the drug completely eliminated ASCVD risk, showing strong reluctance toward preventive medication at low risk which is appropriate. Willingness increased modestly as baseline risk rose: at 10% risk, refusals dropped to 42.9% (U.S.) and 42.4% (Japan); at 20% risk, to 23.6% (U.S.) and 38.4% (Japan).
The median SWD—the required absolute risk reduction—was 7.5% in both countries at 10% baseline risk and 10.0% (U.S.) versus 12.5% (Japan) at 20% risk. This means the public expects a 75% relative risk reduction with statins over two years (baseline risk 10%). These thresholds substantially exceed the true benefit of statins, meaning that most respondents demanded a ten‑fold greater effect than the drug can deliver. Accordingly, only a minority would accept statins at real‑world efficacy: in the U.S., 13.8% at 2% risk, 23.6% at 10% risk, and 34.2% at 20% risk; in Japan, 19.2%, 23.9%, and 30.6%, respectively. Japanese respondents scored lower on comprehension of adverse effects, yet sensitivity testing confirmed similar overall patterns.
Interpretation:
Across both nations, people required substantially larger benefits than statins provide before considering therapy worthwhile. This disconnect suggests that the public values absolute benefit magnitude more than professional guideline writers assume. The similarity between countries, despite differing health systems and ASCVD prevalence, indicates a shared human tendency to weigh small preventive benefits against financial, practical, and perceived safety burdens.
Implications:
The results highlight a persistent gap between patient expectations and what medication can deliver. Integrating SWD analysis into guideline development could enable more transparent, value‑based risk thresholds and improve shared decision‑making. For clinicians, expressing benefits in absolute rather than relative terms may align expectations and foster trust.
Conclusion:
Most adults in both the U.S. and Japan believe statin benefits are insufficient to justify therapy for primary prevention. There is a mismatch between population expectations and real benefits of statins. The public wants more risk reduction than statins can deliver.
Please subscribe to FOCAL POINTS as a paying ($5 monthly) or founder member so we can continue to bring you the truth.
Peter A. McCullough, MD, MPH
President, McCullough Foundation
FOCAL POINTS has partnered with Patriot Mobile to defend your medical freedom. Join Patriot Mobile today!
Reference:
Luo Y, Kawakami H, Funada S, et al. Measuring Public Preferences for Statin Therapy Using the Smallest Worthwhile Difference. JAMA Internal Medicine. Published online February 16, 2026. doi: 10.1001/jamainternmed.2025.7958




Educating people on absolute v. relative risk is very hard to do. And the oldest trick in the book is using one or the other, or both, selectively, “reduces Covid 95%”.
Statins of course are a funny one. As they increase risk of diabetes, cause calcification of the arterial walls, and muscle deterioration that is irreversible. And the actual all cause mortality difference is zero. At best.
Absolute risk reduction is the only number of value, relative risk reduction is a fake-out statistically manipulated number to make people think a drug is far more effective than it actually is, using statistical lies. Older studies put the ARR for statins at 1%, while patients were only advised the RRR of 30%.
The side effects of statins are incredibly severe, including muscle pain and wasting (the heart is a muscle) major cognitive decline and general loss of energy. This is particularly bad for elderly people. I know several people with these terrible side effects ho could not work out and had memory issues on statins, who stopped taking the prescribed drugs and their health improved dramatically with strength and thinking ability vastly improved.
If the only reason for giving a statin is elevated cholesterol, a constantly changing ‘marker’ reduced to an ever lower standard so the drug can be subscribed to more and more people. Statins are the most successful drugs in history with the highest profits for Big Pharma. Do doctors receive incentive or bonus payments for prescribing them to more people, as pediatricians do for having a high percentage of patients on the CDC schedule?
Monetary incentives for prescriptions/ ANY meds needs to be outlawed.
From books I have read on this topic, understand that people die of heart issues with low or high blood cholesterol levels, and in elders higher cholesterol can leave you in a better state of overall health and better longevity than low cholesterol. Our bodies make the cholesterol we need and if this increases with age it protects the brain.
At this point, I refuse all vaccines unless and until true inert-placebo safety and efficacy studies are completed. I refuse all statin drugs. I take large quantities of vitamin D3 and my blood level is about 100 ng/ml. I am 75 years old and my BP is 118/ 70 in the doctors office. Total cholesterol about 200 to 210 for many years.
Everyone needs to research all prescription drugs, vaccines, and vitamins on their own. The healthcare system is hopelessly committed to their standard of care protocols, even if it kills you!
One of my friends was 94 a few years ago, little Italian lady and I asked her why she has such good health. She said, I cook and eat real food, I am very active (walking in the pool, dancing, social activities) and I don’t follow doctors advice much...my kids make me go if I am sick and they always prescribe something. The medicines make me sick to my stomach so I throw them out and lie that I took them. She outlived several of her doctors and is now 99 years old, using a walker and spunky as heck!!