By Peter A. McCullough
Nearly five years after the first fatal cases of mRNA COVID-19 myocarditis were reported to the US public health cases, an NIH NHLIBI funded study at Stanford found a minor part of the formidable mRNA Spike protein induced cardiomyocyte injury after vaccination with Pfizer and Moderna. Liz MacDonald interviewed cardiologist Dr. McCullough on The Evening Edit, FOX Business. This summary was assisted by AlterAI.
Summary: Cao et al, Molecular Mechanisms of Vaccine-Induced Cardiac Inflammation
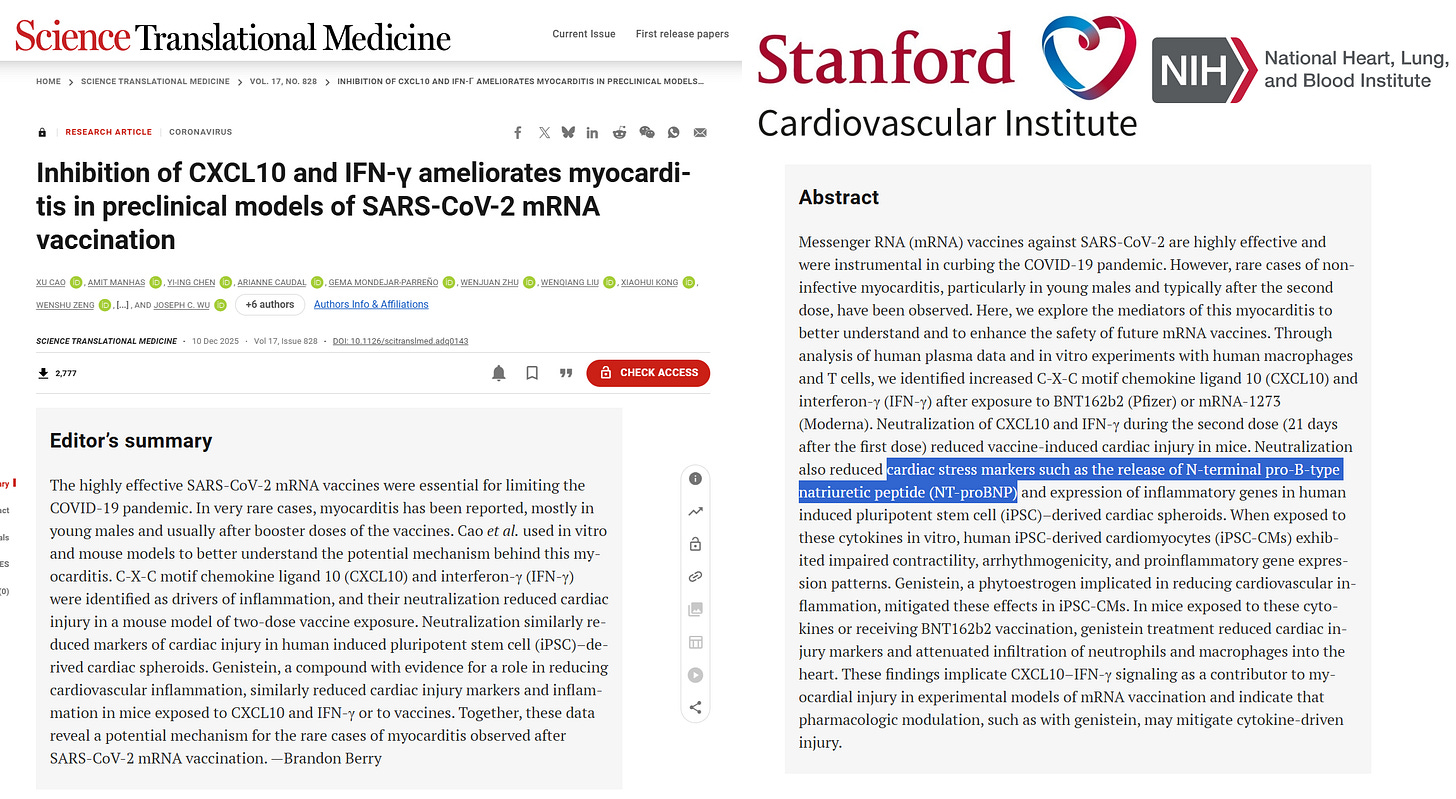
Recent research published in Science Translational Medicine (December 10, 2025) elucidates minor molecular mechanisms underlying vaccine-induced cardiac inflammation, particularly myocarditis observed after mRNA-based COVID-19 vaccination. It is well known that both Pfizer and Moderna mRNA circulate in the bloodstream for months to years. They deposit in the heart and begin production of the damaging and pro-inflammatory Spike protein. Both mRNA and Spike protein trigger a broad range of inflammatory factors, two of which were the subject of the study done at Stanford.
The study identifies a specific immunological pathway — involving CXCL10 and interferon-gamma (IFN-γ) — involved in vaccine-induced inflammation. Vaccine myocarditis is common and the discovery provides a minor mechanistic insight linking mRNA vaccine components to immune-mediated myocardial injury.
The researchers found that certain individuals exhibit an exaggerated two-step immune response following exposure to the Spike protein translated from mRNA vaccines. This begins with a surge in type I interferon signaling and is followed by strong activation of cytotoxic T cells in cardiac tissue. Elevated levels of CXCL10, a chemokine that recruits T cells to muscle tissue, were consistently associated with the onset of myocarditis-like pathology.
In in vitro studies, blocking CXCL10 and IFN-γ signaling prevented muscle cell death and stopped myocarditis in animal models, confirming these molecules’ central role. These findings open a potential therapeutic window for preventing or mitigating vaccine-associated myocarditis—for instance, by transiently inhibiting these cytokine pathways in susceptible patients.
Crucially, the study’s authors emphasize that this immune cascade arises not from contamination or infection, but from a self-amplifying feedback loop between vaccine-loaded dendritic cells and cytotoxic lymphocytes. In certain individuals—especially younger males with elevated testosterone and vigorous innate immune responses—the resulting inflammation overwhelms regulatory mechanisms that normally dampen immune activation in heart tissue.
This dysregulation likely represents a specific maladaptation of the immune response rather than a general reaction to vaccination. However, it may be compounded by genetic predispositions, prior vaccination, or autoantibody presence against cardiac-specific antigens.
This study validates the biological reality of vaccine-induced myocarditis as a genuine immunopathological entity rather than a coincidental statistical anomaly. Second, it provides a molecular target for both diagnostic and therapeutic advances. Detecting elevated CXCL10 or IFN-γ post-vaccination could enable early diagnosis of vaccine heart damage.
Yet the broader significance extends beyond myocarditis. The same cytokine network—IFN-γ and CXCL10 mediated T-cell recruitment—is implicated in autoimmune myocarditis, long COVID, and even post-viral fatigue syndromes. This mechanistic verification exposes the institutional reluctance to acknowledge immune dysregulation risks tied to mRNA vaccine platforms.
While the original authors present their findings in cautious, establishment-friendly language—stressing the overall rarity of severe outcomes—the underlying data point to a clear causal immunological mechanism. This marks a major step toward accountability in biomedical transparency, shifting the conversation from probabilistic associations (“rare events”) to well-defined molecular processes.
Future research will focus on identifying mRNA and Spike protein in cardiomyocytes and cardiac tissue, find biomarkers for susceptibility, and in addition to McCullough Protocol Base Spike Detoxification, therapeutic trials could explore chemokine blockade strategies, and reassessing dosing intervals to reduce cumulative cytokine load.
Ultimately, recognition of even a minor mechanism while ignoring mRNA and Spike protein in the heart, represents both a scientific advance and a test of institutional integrity for the NIH. After years of denial, public health bodies should openly integrate this knowledge into safety policies or continue the pattern of minimizing post-vaccine immunopathology.
Please subscribe to FOCAL POINTS as a paying ($5 monthly) or founder member so we can continue to bring you the truth.
Peter A. McCullough, MD, MPH
President, McCullough Foundation
Reference:
Breindl, A. (2025, December 12). Research unpicks molecular mechanism of vaccine-induced cardiac inflammation. BioWorld Science — summarizing findings from Science Translational Medicine, Vol. 17, Issue 1234, DOI: 10.1126/scitranslmed.adq0143.